The Promise and Perils of Over-the-Counter Birth Control
As Opill hits shelves, more women are also expressing skepticism about hormonal contraceptives. They should be heard.
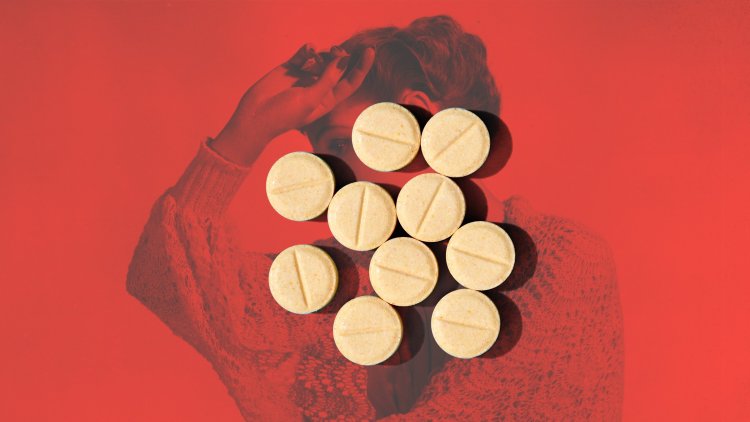
Perhaps you’ve noticed something new at your local market. Opill, the first oral contraceptive approved by the FDA for over-the-counter use, began shipping to U.S. stores in March. It has no age restrictions and does not require a physician’s sign-off; you can now buy a three-month supply at Walmart or Target the same way you might pick up Tylenol or tampons or a six-pack of seltzer.
This is, without a doubt, a momentous development in the realm of reproductive health. In the post-Dobbs environment, in which access to abortion care has been severely restricted across the United States, easier access to contraceptives is significant. Yet Opill also debuts as more and more women, in public forums and in their physicians’ offices, are raising concerns about the effects of hormonal birth control on their physical and mental well-being—and are pushing back against the idea that pharmaceuticals are their best options for trying to prevent pregnancy.
For the past few years, the “Why women are going off the pill” essay has become a staple of lifestyle journalism. A search for birth control on TikTok yields thousands of videos, many taking a negative stance on hormonal methods. Side effects are a common complaint: mood changes, headaches, irregular bleeding, lower libido—or, in some instances, more dangerous complications, such as blood clots. Many of the critiques note that women’s concerns have a history of being overlooked or dismissed by the medical establishment, and that women are still waiting for an improvement on the birth-control status quo.
[Read: The Coming Birth-Control Revolution]
In many spaces, this upsurge in discussion has been treated not with curiosity, but with contempt. Those airing dissatisfaction, or simply describing potential side effects, have been called antifeminist or accused of threatening other women’s birth-control access. Commentary critical of the pill has been dismissed as misinformation by mainstream news outlets—not always unfairly, as much of the material on social media can’t exactly be called reliable. (“Wellness” figures hawking fertility-awareness “coaching” abound, as do right-wing influencers with barely concealed agendas.)
But at the same time, many people online are recounting real stories of real symptoms, and expressing legitimate qualms about the options they’ve been given. Their distrust is not unfounded. Kate Clancy, a biological anthropologist and professor at the University of Illinois at Urbana-Champaign, and the author of Period: The Real Story of Menstruation, told me that women “are very often subject to medical betrayal—to having really awful experiences in a medical context.” Clancy said she was “glad there’s improved access.” But if you already harbor mistrust, “if you already have reasons to say, ‘Wow, these pharmaceuticals were not really made for me,’ then over time I understand why people arrive at a place where they are dissatisfied with current options.”
This is where the tenor and content of the discourse can be vexing: The public takedowns of skeptical women risk silencing the important conversations people ought to be able to have in service of meeting their health-care needs. If women’s overall betterment is the goal, then narrowly prioritizing access—celebrating a development such as Opill while shouting down the women simply trying to talk about their experiences—is counterproductive. To address reproductive health in full, taking into account questions about rights, responsibilities, and the physical and social ramifications of pharmaceutical solutions, requires a wider lens.
A few years ago, I was prescribed an oral contraceptive after a conversation with my doctor that could most generously be described as extremely brief. In the month I took the pill, I was overtaken by a debilitating brain fog that felt like a loss of self. I was irritable, snappish. I made my living as a professional columnist, yet suddenly I felt bad at writing—not in the sense of the usual scribbler’s procrastination, but in that I genuinely couldn’t generate ideas or string together words. I contemplated leaving my job. I cried a lot.
I realized the cause of this identity shift only after my prescription ran out and my regular personality snapped back into place, seemingly overnight. I hadn’t turned into a failure. Hormonal birth control had derailed me.
The pill is something of a catchall term, used to describe a variety of oral contraceptives that make the uterus inhospitable to pregnancy and often prevent ovulation. “Combination” pills, the most common type—and the kind I was prescribed—contain synthetic estrogen and progestin (a synthetic version of the hormone progesterone); “mini-pills,” of which Opill is one, contain progestin alone. Early versions of oral contraceptives had extremely high doses of both hormones, leading to sometimes severe side effects. Newer versions, with more carefully calibrated doses, have lessened, though not eliminated, those risks.
Today, oral contraceptives are the second-most popular birth-control method for women in the United States, after permanent sterilization. Fourteen percent of girls and women ages 15 to 49 use them, according to a federal survey from 2017 to 2019, the latest data available; nearly one in five American girls between the ages of 15 and 19 are on the pill. Over the decades, several studies have found that many people who start taking the pill will eventually go off it because the side effects are so intolerable. Concerns about side effects are also frequently named as a reason women resist taking their “preferred contraceptive method” in the first place.
It is not a stretch to imagine that young women taking an over-the-counter pill, unmonitored, could be left dealing with symptoms they might not be prepared for—without the recourse or the wherewithal to ask questions, or without the knowledge that what they’re experiencing is worthy of concern. Sarah E. Hill, a psychology professor at Texas Christian University and the author of This Is Your Brain on Birth Control: How the Pill Changes Everything, told me she’s in favor of removing barriers to access and supports Opill coming to market. But “I worry about it,” she said. “For everybody, but I worry about it most intensely for adolescents, whose brains are still developing.” Recent studies have found evidence of an increased risk of depression in some of the youngest users of hormonal birth control, and Hill said it troubles her to think about “young women who are most vulnerable to getting these kinds of side effects going on this medication and not being watched.”
Nearly all medications come with potential negative side effects, and we still use them as tools. You can get liver damage from taking too much Tylenol, but in the right amounts, the drug can lower a worrying fever. And in the case of birth control, of course, any adverse effects must be weighed against the life-changing alternative: becoming pregnant, one of the riskiest undertakings many women will ever experience. Forty-six percent of pregnancies in the U.S. are unintended, one of the highest rates among wealthy nations, and the rate tends to be highest among low-income populations and younger women. Those are the same populations most likely to take advantage of a pill that has no age restrictions and does not require a visit with a health-care provider for a prescription and subsequent renewals.
My own disturbing experience was, I know, not a universal one (though there is at least one high-quality study, of more than 1 million Danish women and girls, suggesting a linkage between hormonal birth control—especially progestin-only formulations—and higher rates of depression). And some people decide that even significant side effects are worth it when they desperately want to prevent pregnancy and hormonal birth control is the only, or the most readily accessible, option. Here is where Opill could be transformative—imagine a woman being pressured into pregnancy who can now buy birth control without alerting her partner, or a working mother who doesn’t have the time or resources to meet with a prescribing doctor but can walk to the nearest CVS.
But I do wonder: If I had started taking hormonal birth control unsupervised, as a teen or a young adult, would I have spent my entire adulthood believing my personality to be different than it was? What would that have meant for me—and the trajectory of my life?
It would be an understatement to say that women have put up with a lot in the name of reproductive health, including many discomforts and inconveniences that men have refused to endure, and that the conventions of medical research have allowed them to avoid. This is not to say that efforts have not been made to get men to do their part.
Andrea Tone, a medical historian and professor at McGill University, told me that in the 1960s and early ’70s, “activists clamored for a contraceptive pill for men so that they, too, could share its responsibilities and risks.” Clinical trials for male hormonal birth control began as early as the 1970s. But a 2016 study noted that a trial for a hormonal injection was canceled after men reported side effects, including acne and depression—never mind that for decades, women have endured these afflictions and worse.
[Read: New Male Contraceptives Could Be Infuriatingly Pain-Free and Easy]
In a recent Atlantic article, my colleague Katherine J. Wu detailed current research and potential innovations in male-managed birth control, noting that although the list of contraceptive options available to women has lengthened since the introduction of the pill 64 years ago, most of the changes have been incremental, and women are still left to deal with a wide variety of side effects and inconveniences. In contrast, the medical system seems to bend over backward to ensure male users are comfortable: Experts have said they doubt that the side effects typical of the female contraceptives on the market would be deemed acceptable by evaluators of the clinical trials of male birth-control methods.
Easier access to the pill eliminates real barriers. But in a medical industry that has long centered male comfort when it comes to reproductive health, an undue burden will always be placed on the people capable of becoming pregnant. As Tone put it, “Making pill-based hormonal contraception available OTC normalizes birth control as a female responsibility and, possibly, even an expectation.”
That expectation may very well continue to serve as an excuse for overprescribing, for overlooking women’s concerns, and for failing to hold accountable a health-care system that has historically not served women well. Ease of access is “a really good thing,” Clancy, the University of Illinois professor, told me. “But there are things in addition to contraception we need to be doing to improve the lives of people who can get pregnant, like broader social infrastructure to improve their care.” Instead, she said, “we just choose to kick the can down to the microsolution and make it about individuals making decisions.”
This is where the knee-jerk pushback to discussion of hormonal birth control’s potential downsides becomes harmful. To support individuals, we need more conversation, not less. It should be possible to celebrate increased access to birth control and to validate women’s negative experiences. It should be possible to praise Opill and to push back against the unfair assumption that women must bear the material and physical costs of contraception.
In a 2023 survey of people assigned female at birth, conducted by the reproductive-justice nonprofit Power to Decide, almost a quarter of respondents ages 15 to 19 said that they lacked sufficient information to decide which birth-control method was right for them—a gap that speaks to a larger problem with the American approach to reproductive health. In an ideal world, the health-care providers I spoke with told me, doctors would spend more time with patients, health literacy would be higher, and reproductive responsibility would be shared between women and men. To create such a world would require not only a cultural shift but also a remaking of the American way of providing care—a not-impossible task, but a much heavier lift than selling a pill.
When you buy a book using a link on this page, we receive a commission. Thank you for supporting The Atlantic.
What's Your Reaction?