Here’s why pain might last after persistent urinary tract infections
Experiments in mice reveal that the immune response to a UTI spurs nerve growth in the bladder and lowers the pain threshold.
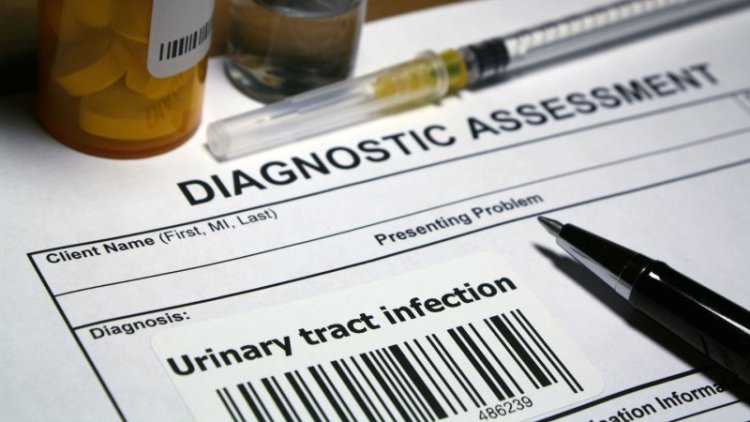
Urinary tract infections are painful, inconvenient and incredibly common. For decades, doctors haven’t had any leads on why, even after several rounds of antibiotics, UTI pain can linger. Now they do.
Nerve growth from immune responses to the infection might be to blame, researchers report March 1 in Science Immunology. Understanding immune and nerve responses to persistent UTIs, the team says, could possibly lead to new, antibiotic-free forms of treatment.
Over half of women will have a UTI in their life, and around a quarter of infections come back within six months. The pain from these infections can be quite difficult to treat, says Marcus Drake, a neurological urologist at Imperial College London. “It’s a ‘heartsink situation’ for the patients, and it’s a heartsink situation for the doctors, because there isn’t much that you can do.”
Puzzled by why pain persisted after UTI-related bacteria were wiped out, immunologist Soman Abraham of Duke University and colleagues collected urine samples from women with recurring infections. Compared with samples of women without recurring UTIs, these showed signs of nerve activation.
To better understand what was happening at the tissue level, the team induced multiple UTIs in mice. Compared with uninfected mice, “we saw a tremendous growth of nerves,” Abraham says. But that only confirmed what the team suspected about humans. The researchers still wanted to know what spurred the nerves to grow.
Abraham knew that when the urinary tract is infected, one of the bladder’s first defenses is to shed a tissue layer to remove bacteria. But in this process, nerves are sloughed off, which jolts nerve-growing immune cells into action. A close look at the bladder tissue of the mice with repeat UTIs revealed an abundance of two kinds of immune cells.
Specifically, there were high levels of mast cells, which are stored in bladder tissue and produce a substance called nerve growth factor (SN: 9/5/07). And there were monocytes, blood-based immune cells that rush to the site of infection to produce even more nerve growth factor (SN: 7/30/09). Similar to respiratory infections, the more often the body has to fight off bladder infections, the better it gets at it; monocytes and mast cells get faster at their job with each UTI. “The unfortunate part is [it becomes] an overzealous response,” Abraham says.
Pain continues because nerve growth factor doesn’t just generate nerve growth; it also lowers the threshold at which nerve pain and pressure receptors activate. Even after no infection-related bacteria remained, the mice in the study had frequent urination and showed signs of lingering pain. “The slightest, innocuous volume of urine was enough to trigger the voiding response,” Abraham says. But with antihistamines and blockers of nerve growth factor, the mice were able to feel some relief.
Right now, persistent pain in UTIs in humans is usually treated with anti-inflammatory or other pain-reducing drugs, including antihistamines, but all of these are a bit unsatisfactory, Drake says. The researchers hope that understanding how nerves grow with recurrent UTIs can lead to more effective pain relief treatments in the future.
What's Your Reaction?